Overhead motion isn’t necessary for everyone, but it’s a good idea to keep it if your clients have it, and try to regain it (where possible) if they’ve lost it. What follows is a “brief” overview of a bunch of contributing factors that can affect shoulder and overhead motion in your clients.
Having control over more motion is always better than having no control over motion, or not having that motion at all. That said, I have a lot of clients for whom going overhead isn’t an option due to injury, degenerative changes, or other fun things that get in the way. This is where goal setting and matching the exercise to the client becomes important--because not everyone needs it and forcing it won’t result in good things.
Overhead motion has a ton of moving parts.
There’s rarely only one keystone that holds people back from getting to a specific position or range of motion, especially so with the shoulder complex. There are a lot of moving parts that create shoulder flexion to get the arm overhead: 12 ribs and their vertebral attachments--10 with sternal attachments; scapular motion through three dimensions (frontal plane, sagittal plane, and transverse plane rotations); humeral rotation and alignment within the glenoid fossa; AC and SC joint motions or limitations; vertebral motion of at least the 12 thoracic vertebral segments; and finally, local muscular issues.
The means to simply get your arms in the air (to wave them like you just don’t care) can take motion from 38 joints through three planes of action, and muscular actions from at least 24 muscles that attach through the thoracic spine, scapula, and humerus.
Assuming your client has relatively normal anatomy--we’re talking no congenital structural issues like scoliosis and degenerative changes disturbing motion abilities, or neural dysfunctions like cerebral palsy--many mechanical issues can be grouped together. In many cases these issues, whether they’re foundational or joint-specific, seem to follow a set pattern.
How breathing plays a role in overhead motion
The main function of breathing is obviously gas exchange, though breathing is sort of a hot button topic in the fitness industry these days. Some people say things like, “I’ve been breathing my whole life and I seem to be doing okay.” Others say, “Do this breathing drill to add 340 pounds to your deadlift today!” Focus on breathing mechanics, however, is not for either of these reasons. It should be more on how that motion of breathing occurs.
We’ve all become pretty good at breathing and not suffocating over the years, but breathing requires a lot of motion from a lot of segments, with assistance from a lot of muscles. Your diaphragm plays a big role in breathing, but don’t forget the intercostals, serratus anterior, rhomboids, rectus and oblique abdominals, transverse, pelvic floor, upper traps and scalenes, subclavian, pec minor, sternalis, erector spinae, sternocleidomastoid, and probably another dozen or so I’m forgetting. Altogether they contribute in varying amounts to breathing depending on how you or a client choose to access lung expansion and depression.
Your client’s position--thoracic extension, flexion, rotation, scapular protraction or retraction, or even a forward head posture--determines whether using some muscles will be easier than using others. If your client chronically holds one position for many years, he begins to automatically rely on those muscles that are used all of the time and pretty much shut down the ones that aren’t. The result is, it becomes difficult to make these muscles work with your client’s positional breathing; but it can also be difficult to make them work in other positions.
According to the law of Specific Adaptation to Imposed Demands (SAID), if you’re consistently in a certain position or posture, your body gets good at being in that position or posture. If you never move from that posture, you’ll likely not be great at moving into other postures either. This makes it challenging to breathe via rib expansion at the sternal attachments or through the ribcage and diaphragm depression. The individual, however, will find other ways.
In order to bring your client’s arms overhead, he has to go through some thoracic extension and rib expansion to allow the shoulder blade sufficient rotation to let the arm actually go overhead, without causing the humerus to butt into the acromion. When bone-to-bone contact happens, movement doesn’t get easier. So if a person’s breathing is keeping him from accessing that thoracic extension and rib expansion, it’s going to hinder his shoulder mobility (which is why it’s the starting point in that series mentioned above).
In a study looking at tetraplegics, De Troyer et al (1986) showed that while they had no use of the diaphragm they could still get comfortable inhalations and exhalations by using the clavicular head of the pectoralis muscle and a large rib flare motion. This simply shows that breathing mechanics can occur from a number of different mechanisms in different people. Having worked with a few spinal cord injured clients, I’m always amazed to see what adaptations can occur.
Rib flare? We can help fix that.
With non-plegic individuals, there’s a form of rib flare, where the positioning of the anterior chest wall almost looks concave instead of convex. As the arms raise up, the ribs don’t expand but simply tilt up:
Mobility through the sternal attachments of the ribs and intercostals seems to be restricted for this pattern, compared to unrestricted free movement:
A much better example of controlled shoulder flexion without rib expansion comes here from Christine Ruffolo:
If someone is getting that massive rib flare motion to substitute for thoracic extension, try to use inhalation movements to create some expansion through the rib cage, which would help prime the person have that motion during shoulder movements.
Consider these breathing drills as mobility exercises, specifically looking at thoracic and sternal motion. If a rib cage is locked down, it’s going to be tough to get enough thoracic extension to allow for sufficient scapular motion. This doesn’t mean pain, just movement that isn’t sufficient for what you want and may lead to mechanical issues downstream.
Breathing drills that reposition your client can help restore some lost motion and set up more successful movements from distal joints. It’s tough for the scapulae to retract and depress if the rib cage is stuck in flexion, and these two movements are effective for getting enough upward rotation to get your client’s arms overhead.
The role of scapular motion in the overhead motion: Is a winged scapula a bad thing?
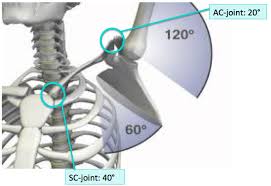
In terms of scapular motion, the shoulder blades have the ability to move through three planes due to their floating attachment to the body. Most of the posterior attachments are through muscular and fascial networks, whereas the only true bony attachment is via the AC joint in the front and the sternoclavicular joint in the center of the chest.
For rotation, the scapulae rely on triangulation force application from three different muscle groups to create upward rotation and produce downward rotation:
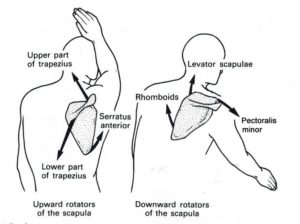
During upward rotation movements, sufficient scapulohumeral rhythm (relation of how much rotation occurs at the shoulder blade versus at the humerus) should be 2:1, where the humerus moves two degrees for every degree that the scapula rotates. For reference, in an ideal world when the arm is overhead at 180 degrees of flexion, the scapula should be rotated to 60 degrees (180-60 = 120, which maintains the 2:1 ratio).
People get into trouble when that scapular rotation doesn’t happen and they wind up shrugging the shoulder to get it into place, essentially substituting side bending at the torso for scapular motion. There could also be adhesive changes in the shoulder joint itself, a condition commonly known as frozen shoulder. In this instance, the rhythm goes from 2:1 down to 1:1, where pretty much all of the movement comes from the shoulder blade and none comes from the humerus itself.
Aside from upward and downward rotation, there’s also forward and backward tilting. Forward tilt is also commonly called winging scapula.

By itself, a winged scapula isn’t a problem, but it is a graphic example of a shoulder that may not have positional strength or stability to get the blade flat to the spine. In order to find stability, the shoulder blade winds up peeling off the torso and angling forward, making it difficult to adequately retract or rotate. Everyone wings in some position or another, it’s a matter of how much and whether it’s a problem or a solution.
Typically, improving “winging” involves directly training the serratus anterior to help promote protraction, but in my experience the serratus isn’t weak, just constantly on. As a result, you can barely palpate the lower traps and rhomboids because they’re fairly atrophied. In many ways, a winging scapula isn’t a single muscular problem, but a systemic compensation. Pretty much all of the muscles that are attached to the scapula need to be strengthened to help regain that torso-hugging position again.
If the goal is to improve strength and stability through the shoulders, a winged scapula might have to be identified and addressed to see significant gains. This just illustrates the rotational capability of the shoulder blade outside of upward or downward rotation. This type of tilting works through the transverse plane in relation to the torso, but there’s also sagittal tilting where the shoulder blade sort of leans over the top of the shoulders, like a weird, creepy Yoda backpack.
This is common with people who have significant thoracic rounding into kyphosis, as well as a forward head posture. It’s challenging to do anything with the shoulder blades other than elevate and protract in this position without addressing thoracic motion first. Hence breathing mechanics work to try to pull them away from the flexion bias and push them towards more extension positional aptitude.
Getting the shoulder blade to move better
A lot of these motions can be helped or hindered through common muscle training and posture work, but some is affected through degenerative or injurious tendencies through the AC joint and SC joint. Having worked with a number of hockey players who all seem to have bilateral AC separations, I’ve observed that their upward rotation is significantly impaired and often not something that can be restored, or even needs to be restored. Not too many hockey players put their arms over their head, except when they score a goal. (I live in Oilers country, so...)
Many people with degenerative issues like arthritis tend to also develop some significant reductions in movement capability via the SC joint. When healthy, it should be able to rotate, elevate, and protract relatively easily. If it’s stuck, the shoulder blade won’t move. Most people won’t have to worry about this unless they’re over 50 and have been stuck in a cubicle for the past 30 years with no other physical activity; or they played a sport with a significant amount of stress on the SC joint.
There are many different ways to get the shoulder to move again. Make it move through the basic patterns of protraction, retraction, elevation, depression, and upward and downward rotation, and you’ll have your bases covered. Just make sure the movement is in the direction you want for your client and not some other Frankenstein direction to simply get the job done.
Here’s some protraction and retraction:
https://www.instagram.com/p/BEPGnhGriCi/
Here’s Cressey talking about getting some scapular rotation via a wall slide:
And here’s retraction and depression:
You could do any of these exercises, or different ones if you want, as long as the movements help your client. If your client can’t get a specific movement to work, spend some more time on it, especially if that movement is important to any activity he wants to do. If you can’t get that movement because of a locked-up thoracic spine or poor positioning to accommodate the movement, spend some time adjusting your client’s thoracic positioning and mobility to allow an easier time to access those movements.
Assessing your client’s upper body movement and solutions
Look at the thoracic spine prior to starting any of the scapular movements. A rounded thoracic spine will make retraction and rotation difficult. A hyperextended spine will make elevation and protraction difficult. Get your client into a position where the movement can be done with less restrictions, and you’ll win.
If a movement is troublesome, but is important for your client’s goal activities, do more of it until it gets easier. If your client just can’t do it, there are a ton of regressions you could go through, but use what works to produce the movement you want. The lat muscle, for instance, causes the humerus to extend and externally rotate, and pulls the scapula into retraction and depression. If your client does a row and his shoulder blade winds up in his ear with the hand on his chest and elbow out in the boonies away from his body, he’s not using his lat. Do you want him to use his lat? Yes, you do, especially when doing a row. Adjust how those shoulders move and redo the thing to get the benefit you’re after.
Next, look at glenohumeral motion. The basic stuff to check are external rotation and internal rotation, as well as both rotations through specific positions, such as with the arm abducted, adducted, or wherever your client needs to have rotational control. If you want to do muscle testing on the muscles controlling these motions, have at it.
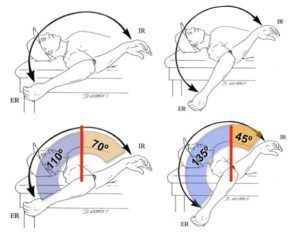
In many cases, the total motion of the shoulder will add up to 180 degrees between both internal and external motion. In some specific populations like overhead throwers, they may have considerably more external rotation and less internal rotation, but the total motion still add up to 180 degrees. In some instances, a person might have more or less, which is cool, but then it comes down to whether the individual needs more motion in the specific direction to do what they want to do.
If your client is a pitcher, for example, he’ll need plenty of external rotation. If she’s an office worker in her 50s, not so much. Someone with frozen shoulders may not be able to get more than a total motion of 90 degrees.
Positioning of the scapula will go a long way toward seeing what range of motion a person can have in his or her GH joint. A retracted shoulder tends to allow much more external rotation, whereas a scapula hanging out in more of a protracted position won’t allow as much external rotation, but might accommodate more internal rotation.
If your client is someone who just wants to lift stuff in the gym and stay fit, but doesn’t have the external rotation through her shoulders to do something like a back squat, it’s going to be challenging to do that exercise without causing some shoulder irritation. Working on shoulder mobility through this motion can help a lot, and in some cases, won’t benefit her too much. Here finding workarounds to perform the exercise can be handy. This is one of the reasons safety squat bars have become popular.
My gym doesn’t have a safety squat bar, and if you’re in a similar situation, you can MacGyver a bar with a bar pad and a couple of towels, as long as the loading isn’t too aggressive.
https://www.instagram.com/p/7fiUY1riAk/
A great benefit to the safety squat bar is it has a camber on either end that sets the weight slightly forward of where the bar contacts the shoulders, making it easier to balance on your shoulders than a straight bar. So if possible, opt for that versus my MacGyvered version, especially if you’re going to rock anything near maximal weight.
Pressing a bar overhead requires a fair amount of GH internal rotation (side note: when biceps wind up pointing towards ears, it’s internal rotation). Bench pressing requires similar internal rotation. To squat, have your client do lat pull-downs behind the head or thumbs up rear delt raises to emphasize more external rotation. This goes to show that understanding what movements your clients have control over and available can make a difference in your exercise selection and relative risk of injury with each exercise.
Here are some simple ways to get some more external and internal rotation. Again, they’re not the only ways, but they are some ways:
Some of these are obviously going to be assisted by a therapist. As a trainer, understand your limits and don’t try to crank on a joint without knowing what you’re doing.
The bottom-line, always start with looking at breathing mobility. Then proceed to thoracic positioning, scapular motion, and finally, look at glenohumeral motion when dealing with tricky shoulder movements that just aren’t giving you what you want. Looking at the shoulder first but forgetting what could be driving its position likely won’t help the problem, so start it from the bottom, just like Drake.
------
This blog post originally appeared on Deansomerset.com. It has been reposted here on The PTDC with permission.