Those of us who have participated in track and field, soccer, football, and sports of a similar nature know the pain and frustration that are shin splints. Thankfully, shin splints are not serious, but they could progress to more serious complications if not treated properly.
If you work with athletes and very active individuals, you may find yourself working with clients who insist on continuing activity, despite the pain. In those cases, you'll have to be prepared with a program to help a client manage and treat his or her shin splints. Here's how.
Shin splints can keep coming back if not properly addressed.
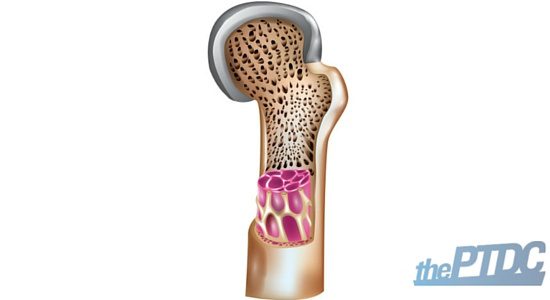
Shin splints are no fun. Their more technical name is medial tibial stress syndrome (MTSS). It's a chronic injury on the medial (inside part), mid-to-lower-third portion of the lower leg. The pain is often described as a dull ache to a fire-like burn that is commonly felt during or after activity.
The types of sports that put athletes at risk include:
- running
- basketball
- tennis
- soccer
- hiking
- jumping
- dancing
- military training
Often, the cause of MTSS is multi-factorial and involves movement dysfunctions, training errors, and various biomechanics-related abnormalities.
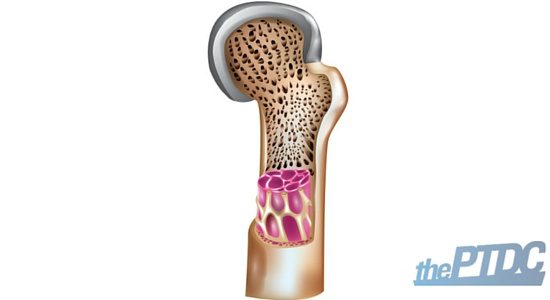
Typically it's an irritation of the periosteum on the tibia (think of it as the saran wrap around the shin).
In general, many experts agree that MTSS is associated with overuse or overtraining from poor foot and leg biomechanics. The popular belief is that shin splints is provoked by poor shoes, training intensity, or bad training surfaces. A critical review called published in 2009 in Sports Medicine that found no grounds for that belief. In reality, it could be any number of things, including:
- Overpronation of the feet
- Oversupination of the feet
- Inappropriate footwear
- Increasing training too quickly
- Running on hard or angled surfaces
- Decreased flexibility at the ankle joint
- Poor knee flexion alignment
- Poor buttock control at in the stance phase
- Poor core stability
- Tight calf muscles, hamstrings
- Weak quadriceps, foot arch muscles
These movement patterns and muscle imbalances can be usually identified with a movement assessment, or a biomechanical analysis of your client's body. Sometimes their therapist can help to correct key dysfunctions in their movement by correcting abnormalities of the spine, SI joint, pelvis, and various muscles imbalances throughout the body.
Our goal with manual treatment is to restore normal range of motion in joints, improve symmetry of muscles and soft tissues, and ultimately, restore maximal function of the body as a unit. To that end, correcting musculoskeletal dysfunctions can improve pain and overall function, and may be helpful in preventing recurrence.
Critical steps to helping your client with shin splints
When someone walks into my office with shin splints, I find that they have muscles that are overactive and under-active. The overactive muscles are doing all of the work while the under-active ones aren't pulling their weight.

Overactive muscles (a.k.a. the control freaks)
- Lateral (outside) calf
- Biceps femoris (outside hamstring)
- Groin muscles
- Hip flexors and TFL
Under-active muscles (a.k.a. lazy bastards)
- Medial calf
- Anterior/posterior tibialis
- Medial hamstrings
- Gluteal complex (max and medius)
Essentially, shin splints are a tug of war in the body, a battle which the overactive muscles are winning. If that's the case, then the solution is simple: give the advantage to the under-active muscles in three "easy" steps.
Step 1: Turn off overactive muscles.
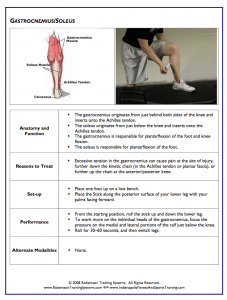
Use self-myofascial release on the gastrocnemius/soleus, adductors, TFL and IT band, and hip flexors.
Foam rolling is one method. I prefer a tennis ball or lacrosse ball. Both are lightweight, can pinpoint specific spots, and are compact enough for travel convenience. Personally, I find rolling on the spot for a few minutes helps relieve the tension and helps you feel "loose". If it's more tender, a minute will suffice.
 Self-myofascial release exercises include calf release on a ball, hip adductor release on a foam roller, hip flexor release on a tennis ball, and thigh release on a foam roller. (Don't worry, I'll have these laid out for you on a sheet below.)
Self-myofascial release exercises include calf release on a ball, hip adductor release on a foam roller, hip flexor release on a tennis ball, and thigh release on a foam roller. (Don't worry, I'll have these laid out for you on a sheet below.)
Coach Jon interlude - A Bonus:
Mike Robertson has given the PTDC permission to give away free copies of his guide Self Myofascial Release Purpose Methods and Techniques. Before I knew Mike I used this guide daily in my training. It's a fantastic Ebook complete with instructions on foam rolling bodyparts and instructions.
I used to print out whatever pages my clients needed and staple a little book for them to use as part of their warmup and suggest that you do the same. Simply click on the book below to download it straight to your computer.
(Note: It's an automatic download so you may want to right click and select "save link as" to save it to a specific destination on your computer)
Step 2. Elongate the short muscles.
Lengthen the overactive muscles with static stretching. Most experts recommend stretching for a maximum of 30 seconds for 1-2 sets to achieve what we want here.
Some exercises include a calf stretch against the wall, hip abductor (or ITB) side-lying stretch, hip flexor stretch, and hip adductor stretch.
Step 3. Turn on the lazy muscles.
Turn on the under-active muscles with isolated strengthening in the following muscles:
- Posterior tibialis
- Anterior tibialis
- Glute medius
- Glute maximus
- Lateral tube
You can do ankle inversion and dorsiflexion eccentric exercises with a band, banded clamshells, side stepping with a band at the knees, and so on.
To make things easier, I've provided a full program you can give your client to correct movement dysfunction and eliminate shin pain (along with other lower extremity problems, such as "runner's knee", Achille's problems, and hip or lower back pain). You can download the template here for free.
 It's pretty common practice to do a regimen of calf stretching and eccentric calf exercises to prevent muscle fatigue daily, or even multiple times a day. Another focus is on strengthening the tibialis anterior and other muscles that control the foot.
It's pretty common practice to do a regimen of calf stretching and eccentric calf exercises to prevent muscle fatigue daily, or even multiple times a day. Another focus is on strengthening the tibialis anterior and other muscles that control the foot.
Work on increasing strength in the abdominals and glutes to improve your client's running mechanics and prevent lower-extremity overuse-related injuries. Your client may also benefit from strengthening the core and hip musculature.
Basically, developing overall muscular strength will improve endurance, but it would be best to wait until your client is out of the "acute" phase of the shin splints injury.
Some points to remember about your client with shin splints
When your client's physical therapist or doctor has ruled out other serious possibilities (like a stress fracture), you can help him or her fix these problems with a flexibility and strengthening program, like a sample one I've provided at the link earlier.
If you're dealing with a fresh injury, advise your client to rest and avoid doing anything that would agitate the injury.
"Rest" in this instance means to do things like riding a bike, swimming, or going on the elliptical, not simply sitting on the couch.
Once the pain subsides, help your client modify his training routine and address biomechanical abnormalities. In addition, keep these points in mind:
- Less activity: Decrease weekly running distance, frequency, and intensity by 50 percent. This will likely improve symptoms without complete cessation of activity.
- More stable surfaces: Synthetic track or a uniform surface of moderate firmness provides more shock absorption and causes less strain on the feet.
- Try proprioceptive training: Proprioceptive training is great for training the nervous system to work well with the muscles. There're lots of ways to do this: standing on one leg, on wobble boards, or on balance boards are some examples. Improving your client's proprioception increases the postural stabilizing muscles to help his body react to the different running surfaces and preventing re-injury rates.

Afterward, over a period of weeks, your client may slowly increase his training intensity and duration while adding sport-specific activities, jumping exercises, and even hill running to the program. The key is being pain free. If your client experiences pain, dial back the exercises.
Bottom-line: shin splints don't mean an end to training. Rather, they're preventable and fixable as long as you help address the problem with diligence, patience, and the right protocol.
Other Articles That Trainers Found Helpful
- Why People Must Squat Differently By Ryan DeBell
- Upper Crossed Syndrome: A Personal Trainer's Guide By Eirik Garnas
- 5 Steps for Dealing With Anterior Pelvic Tilt By Eirik Garnas
Photo Credit: Pexels.com, Wikimedia.