Obesity and diabetes are growing problems all over the world. These two health conditions often go hand in hand, but they’re not mutually exclusive. According to the International Federation of Diabetes, at least 415 million people suffered from diabetes in 2015. This number is expected to rise to 642 million by 2040.
That’s a serious problem.
As personal trainers, we can play a key role in promoting a healthier way of living for our clients, as well as assist with the management and prevention of diabetes. It all starts with proper education.
Diabetes 101: Know how to help your client with diabetes.
Diabetes is a complex disease. One of the most celebrated Greek physicians, Aretaeus of Cappadocia, described diabetes as a “melting down of flesh and limbs into the urine.” It sounds morbid, but that’s a fairly accurate description.
There are two main types of diabetes: type 1 and type 2. They’re both related to impaired glucose control, but the difference is in the onset of the disease.
* Type 1 diabetes is an autoimmune condition that’s associated with genetic defects, intestinal permeability (leaky gut), and environmental triggers, such as infections and viruses.
* Type 2 diabetes is a chronic metabolic condition that is characterized by insulin resistance (that is, the body's inability to effectively use insulin) in combination with insufficient insulin production by the pancreas. Together this results in high blood glucose levels (hyperglycemia). Type 2 diabetes is commonly associated with obesity and physical inactivity.
Medication is important in the treatment of type 1 and serious cases of type 2 diabetes. Both conditions require serious lifestyle modifications for proper long-term management. So what are the best preventative and treatment measures? As you probably guessed, it’s diet and exercise.
Diet and exercise are useful in treating both forms of diabetes. But while exercise provides a wide range of health benefits, it can also present a number of challenges to the client suffering from diabetes.
For those living with type 1 diabetes:
These clients use insulin to help manage glucose levels. However, using injectable insulin increases the risk of hypoglycemia (low blood sugar), which, in turn, makes it difficult for the client to perform and also dramatically increases the risk of injury. Other side effects include reduced cognition, nausea, and sudden muscle weakness. One thing to note is, low-intensity cardio poses a greater risk for hypoglycemia (high blood sugar) than higher intensity exercise.
High-intensity exercise, on the other hand, increases stress hormone production (cortisol, adrenaline, and others), which increases blood glucose levels. Since type 1 diabetics are deficient in insulin, they lack the ability to process this newly produced glucose. As such, hyperglycemia is a common problem with higher intensity forms of exercise.
It's important to understand the diabetic body’s response to high-intensity exercise and correct rising blood glucose levels with necessary amounts of insulin as, and when, required.
For those living with type 2 diabetes:
These clients may have other health complications, such as extremely low levels of physical fitness, high blood pressure, history of cardiovascular disease, obesity, un-healed ulcerations of the foot, or limb amputation.
All of these factors must be taken into account when designing exercise regimens for people with diabetes. Furthermore, issues with exercise advice for patients living with diabetes is compounded by the fact that most general doctors don’t understand exercise physiology. Further still, diet itself can be a beast of a topic since general advice tends to be tailored toward people who don’t exercise; and many Registered Dietitians also don’t thoroughly understand sports nutrition and its role in diabetes.
ALSO READ: Can Personal Trainers Give Diet and Nutrition Advice to Clients?
Bottom-line, you have a lot of work ahead of you to help clients who have diabetes but want to shred fat, pack on quality muscle mass, and smash personal bests in the gym.
Your role as a trainer is not to diagnose or treat clients with diabetes.
As a fitness professional, you will undoubtedly come across people with either type 1 or type 2 diabetes.
Whatever the case, your help starts with a deep-rooted understanding of the physiological changes that can impact clients living with diabetes when you prescribe them diet and exercise strategies.
Each and every personal trainer has a responsibility to ground their coaching on solid principles that prioritize the health and well-being of their clients. That said, you should avoid making suggestions about a client’s medication unless you are fully qualified and insured to do so.
Coaching etiquette: What you say or do matters
First of all, be mindful of how you communicate to clients suffering from diabetes. Your client probably won’t appreciate jokes about eating sweets and sugar, which are often cracked by family members and friends. The last thing they need is a mentor joking about and making fun of their condition.
Also, labelling a client as a ‘diabetic’ is not regarded as appropriate, especially in the United States. Refer to your clients as “people living with diabetes.” This is a much more subtle way of communicating their identity, rather than branding them as a diseased ‘diabetic.’ I personally hate being called diabetic.
Similarly, when working with the younger generation, choose your words wisely. Avoid language that implies them being ‘overweight’ or in any way discusses unacceptable body shape or size. Instead emphasize gaining health, managing blood glucose, fueling performance, and training appropriately.
4 important things to know about training clients with diabetes
In order to provide the safest and most effective coaching to clients with diabetes, you must understand and respect the following issues.
1. Energy systems and fuel metabolism during physical activity/exercise
People living with diabetes have a reduced ability to match glucose production with glucose utilization, and as such, may need to adjust medication to accommodate. Blood glucose levels can change during and after physical activity or exercise. These changes are largely dependent on the type of exercise performed.

Low-level physical activities, like arm chair aerobics or slow walking, will burn energy, but their effect on blood glucose will be minimal. Moderate-level activities like brisk walking, light jogging, and cycling have a greater potential to lower blood glucose and cause hypoglycemia (depending on how diabetes is treated).
High-intensity exercise, like weight training or interval training, may result in transient hyperglycemia because the liver (hepatic) glucose output tends to exceed muscular glucose uptake, particularly post-exercise.
Consequently, the two main problems with exercise and diabetes are hypoglycemia (low blood glucose) and hyperglycemia (high blood glucose).
2. Monitoring blood glucose
Monitoring blood glucose levels is an essential management strategy for anyone living with diabetes.
Personal trainers should actively encourage diabetic clients to test regularly and ascertain the effect of exercise on their blood glucose control. While a personal trainer's advice on diet and medication is limited, it's relatively easy to access average blood glucose levels during the client's training period.
All blood glucose testing devices come with an average summary button. Simply press it and correlate their average reading with key targets. The table below is taken from the 2016 American Diabetes Standards of Care Strategy. Both UK and International Units are provided.
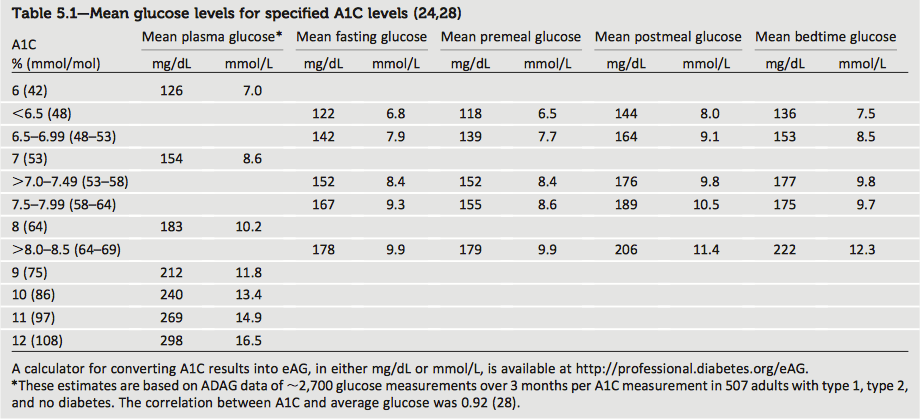
Using this data allows you to see how the exercise program affects their blood glucose management. Assess blood glucose results by looking at the average results from the last few days or some other set time period since starting.
If low blood glucose, or hypoglycemia, is reported frequently, there is a high probability the client may be overeating calories to treat his or her condition. This obviously has implications for fat loss and body weight management.
If hyperglycemia is reported frequently, it could suggest impairments in the client’s recovery and performance. Recall that hyperglycemia is a catabolic condition that increases muscle protein breakdown and promotes dehydration, a key limiting factor in exercise performance. Long-term hyperglycemia has been linked to joint stiffness, foot problems, amputation, and muscular weakness, all of which can affect individual exercise prescriptions.
The data obtained from their blood glucose monitor should always be discussed with their health care team and used to fine-tune diet, insulin dose, and other medications for the best exercise experience possible.
3. Acknowledge different elements of the client’s health care team.
Typically, a client with diabetes has a health care team that he or she sees regularly to help manage his or her condition. Since you would also be involved, you must work together with the client’s health care team. First, obtain a client’s permission to contact members of his or her team. Introduce yourself and relay feedback that would be relevant to the control of the client’s diabetes, body composition changes, illness, injury rehab, and other factors.
4. Respect Your Scope of Practice
There is a clear line that separates a personal trainer from others working outside their scope of practice. Unfortunately, many personal trainers are naïve and take on more than they can chew. This can be due to ignorance, or in many cases, a passion to self-experiment and help others.
Refrain from advising clients on topics you are not qualified to work with, including (but not limited to) diet, medication, depression, and other underlying health complications or injuries.
Helping a client with diabetes is a group effort
The harsh reality is not many medical professionals know how to prescribe exercise for diabetic fitness management. While they are essential to providing a diagnosis, evaluation of blood work during treatment, and prescription of necessary medication, they are unlikely to have had the required training to make effective exercise prescriptions.
You as a qualified fitness trainer must work in unison with a medical professional to promote the most effective exercise strategy for your diabetic clients. Each person’s exercise regime should be modified according to his/her habitual physical activity, physical function, health status, exercise responses, and stated goals.
The same goes for nutrition. Dietary requirements should be adjusted for individuals pursuing different exercise goals and volume. This requires the advice of a qualified clinical and sports nutritionist.
In other words, respect your scope of practice.
If you wish to learn more about diabetes and exercise, make sure to check my content at www.diabeticmuscleandfitness.com.
Photo Credit: Featured Image by Wikimedia, Image 1 by Stock Unlimited images, Image 2 by Stock Unlimited images.